Community Health Centers (CHCs), also called Federally Qualified Health Centers (FQHCs), may be our nation’s best health policy experiment, delivering a bold return on investment in the sixty years since their inception. Every $1 invested in primary care returns $13 in saved downstream costs. From urban areas to rural communities, CHCs play a crucial role in delivering affordable, high-quality primary care for nearly 34 million people across the U.S. They serve patients regardless of insurance status or ability to pay, reducing barriers to care in medically underserved areas like rural communities. They also are job creators, supporting 326,000 full-time jobs across the country. But these outcomes take resources. How are community health centers funded?
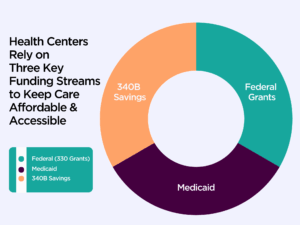
Every CHC is different, but they generally have a diverse funding model that combines core funding into a model to keep programs running. Each health center may rely more or less on a particular funding stream. What’s clear is that, because of the patchwork nature of the funding, reductions in any one of the revenue streams can put CHCs and their patients at risk. Understanding the core CHC funding mix is important as policymakers consider funding appropriations that can strengthen health centers and keep their doors open.
Three Main Funding Sources for Community Health Centers
Federal Government Grants (HRSA Section 330 Funding)
Federal grants are a crucial source of CHC funding. Through Section 330 grants that are funded through discretionary and mandatory Congressional funding streams and managed by the Health Resources and Services Administration (HRSA), health centers receive core operating dollars that enable them to:
- Offer care to all patients, regardless of ability to pay.
- Maintain a sliding fee scale for patients.
- Expand services such as dental care, mental health treatment, and pharmacy support.
- Build capacity for community health initiatives like mobile van health and street or backpack medicine.
These grants act as an important piece of CHCs’ financial foundation, allowing them to stay mission-driven even during economic downturns.
Medicaid
A significant portion of CHC revenue comes from Medicaid, the federal/state and local health insurance program for children and adults who are low-income or disabled. CHCs are reimbursed under a Prospective Payment System (PPS), which is designed to reflect the true cost of delivering comprehensive care to underserved populations.
340B Program Savings
CHCs participate in the federal 340B Drug Pricing Program, which allows them to buy outpatient prescription drugs at discounted rates. This is not a direct funding stream, but a savings stream generated through the 340B program that must be reinvested back into care delivery at the CHC. This program is no cost to taxpayers and in 2023, CHCs accounted for just 5.4% of overall 340B program purchases.
Many CHCs use these reinvested dollars to:
- Provide discounted or free medications to uninsured and underinsured patients.
- Expand in-house pharmacy services and access.
- Fund other essential services like mammography, maternal health programs, patient care coordination, or transportation.
- Support uncompensated or charity care.
For many health centers, 340B savings are a lifeline that helps fill gaps left by limited Medicaid reimbursement rates, stagnant federal funding, or rising operational costs. The hard reality is that federal funding has not kept pace with inflation for CHCs. Unlike traditional or for-profit hospital systems, CHCs cannot upcharge to cover gaps in purchasing power. That means when accounting for inflation, CHCs have less funding per patient than before (see Chart 1), going from $138.16 per patient in 2020 to just $106.83 per patient in 2024.
Why CHC Funding Matters
While some CHCs may receive modest revenue from private insurance, patient fees, and other sources like philanthropic grants, for most CHCs, Medicaid, federal 330 grants, and 340B savings make up the majority of their support, enabling them to serve patients effectively.
This financing model makes CHCs financially viable — but it also means they are vulnerable when one or more funding streams are cut. With not enough federal funding, big cuts to Medicaid, and the continued erosion of the 340B program, our nation’s largest primary care network and its patients are at risk. Your advocacy matters and can help play a part in ensuring that the care CHCs provide remains affordable and accessible.